Australia’s ageing population means that more Australians are getting hip replacements and the good news is that with improving surgery techniques and rehabilitation protocols, Australia has a high rate of hip replacement success. So, what are the keys to having heathy hips and successful hip replacement recovery? In this article we explore how the hips work, how to improve hip health and how to prepare for and manage hip replacement surgery and recuperation.
What are hips and what do they do?
The acetabulofemoral joint commonly known as the hip joint, are ball-and-socket joints located at the junction of the thigh bone and pelvis. They play a crucial role in various movements and are among the largest joints in the body, supporting a significant portion of a person’s body weight.
Hips enable a broad spectrum of movement in the legs, facilitating activities such as walking, squatting, jumping, ascending and descending stairs, sitting, and any other motion that requires lifting or lowering the leg. Ball-and-socket joints like the hips typically exhibit the highest degree of mobility among all body joints.
The hip joint enables various movements such as flexing and extending the legs, rotating them inwards and outwards, and moving them towards or away from the midline. Despite not having an extensive range of motion, it plays a crucial role in stabilising the connection between the upper and lower body.
The anatomy of hips
Hip Bones:
The bones are commonly known as the pelvis. Within the pelvis, two key components play a crucial role in the hip joint; The acetabulum serves as the socket where the upper part of the femur is inserted, while the sacrum provides support to the lower spine and acts as a connection point for numerous muscles and ligaments that help support the hips.
Muscles of the hip:
The muscles of the hip play a crucial role in both motion and stabilisation, with some performing both functions simultaneously. While over fifteen muscles contribute to hip movement, the following are among the largest and most significant:
The gluteus maximus muscle attaches to the ilium, the largest part of the pelvis, and the sacrum. Its primary functions include leg extension and external rotation. This muscle is crucial for actions such as rising from a seated position, running, and walking uphill. Additionally, it plays a key role in supporting the pelvis and enabling activities like maintaining balance on one leg.
The gluteus medius is the main muscle responsible for hip abduction, which involves moving your leg away from your midline. It also plays a crucial role in stabilising your knee when you need to balance on one leg temporarily while walking or running. Positioned between the gluteus maximus and gluteus minimus, the gluteus medius is essential for maintaining proper hip function and stability.
The gluteus minimus is the smallest muscle in the glute group, attached to the ilium. Its primary function is to assist with abduction, but its main role is to provide stability to the hips during these movements.

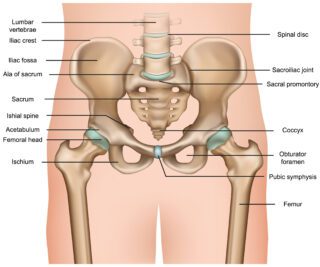
Pelvis Anatomy including the Hip
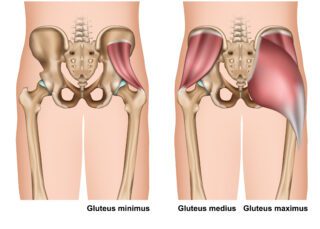
Gluteus Muscles
The psoas major muscle is a significant muscle that connects the spine to the inner pelvis. It plays a crucial role in linking the upper and lower body and stabilising this connection. Additionally, it connects the front of the body to the back. At the hip joint, the psoas assists in leg movement, hip rotation, and provides stability during subtle hip movements.
The iliacus muscle connects the ilium of the pelvis to the sacrum. It plays a key role in leg extension and external rotation.
The piriformis muscle attaches to the sacrum and plays a crucial role in lifting and rotating your leg. It is vital for redistributing your body weight when walking from one side to another.
Nerves of the hip:
The nerves located in the hip region play a crucial role in providing sensation to your legs and facilitating essential functions such as walking and everyday movements. These nerves encompass:
The obturator nerve which supplies sensory innervation to a part of the thigh and serves as a motor input for various crucial hip muscles.
The genitofemoral nerve supplies sensory innervation to the genital area and the lateral femoral cutaneous nerve supplies sensory innervation to the lateral thigh.
The femoral nerve supplies feeling to parts of the leg and controls the movement of the psoas muscle and other significant muscles while the posterior femoral cutaneous nerve supplies feeling to the rear of your thigh.
Sciatic nerve: In certain individuals, this nerve travels above the piriformis muscle, while in others, it goes through the muscle. It plays a role in the movement of your hamstrings. Read our blog about sciatica.
Indicators of potential hip issues
The hip joints are susceptible to both gradual deterioration and sudden trauma. If you experience hip pain or stiffness, these are typically the primary indicators that there may be an underlying issue with your hip. Contact a doctor immediately or visit a hospital emergency department if any of the following occur:
- You cannot move your leg or hip or you cannot stand or bear weight on a leg
- You have intense or referred pain in your hip or leg
- Your hip or leg looks deformed
- Your leg is very swollen or has become swollen suddenly
- There is redness around your hip.
Conditions affecting the hips
Arthritis is a prevalent hip condition where the cartilage in the joint deteriorates over time due to usage, leading to bone-on-bone contact, resulting in pain and limited mobility. Treatment options for hip arthritis typically involve physical therapy, anti-inflammatory drugs, and corticosteroid injections. In severe cases, hip replacement surgery may be a necessary option.
Bursitis is characterised by inflammation of the small sacs of fluid that cushion the joints. The treatments for hip bursitis are akin to those prescribed for arthritis. These may include anti-inflammatory medications, corticosteroid injections, and physical therapy. Lifestyle adjustments to avoid activities that aggravate the hip can also be beneficial. In cases where these methods prove ineffective, surgical removal of the affected bursa may be recommended by your doctor.
Avascular necrosis occurs when tissue in the hip dies due to a lack of blood flow, typically caused by injury or tumours. This can lead to the development of tiny fractures in the hip over a period of months or years, eventually resulting in bone breakdown. The primary symptom of avascular necrosis is progressive hip pain.
Ensure your hip health with these tips:
- Work on improving your posture and maintain a healthy weight
- Take breaks from prolonged sitting
- Strengthen your core muscles, including your glutes
- Avoid high-impact exercises initially and opt for lower-impact movements
- If you experience pain in your hips, rest and ice packs may provide some relief, but don’t delay in seeing your doctor if pain persists
- Early intervention is key to preventing potential complications in the future
Hip replacement surgery rehab and prehab
Re-hab
Physiotherapy following a hip replacement can expedite your recovery process. Ideally, it is advisable to consult with one of our physios prior to surgery as well. Physiotherapists are valuable in overseeing and supporting the rehabilitation journey post hip replacement. We develop precise evaluations and personalised programs that align with your functional capacity and facilitate the accomplishment of targeted objectives in a secure and effective manner.
Pre-hab
Physiotherapy before undergoing surgery helps to ensure that you maintain muscle strength and range of motion in your joints. Referred to as pre-hab, this practice has been shown to reduce complications and enhance recovery outcomes.
Through pre-hab, you will be educated on movements to avoid post-surgery and be introduced to targeted strengthening exercises for the muscles surrounding the hip joint. Hydrotherapy, which we offer at our Runaway Bay clinic, may also be recommended, offering a beneficial way to experience movement, alleviate pain, and potentially facilitate weight loss prior to the surgery.
Whether you want to get in shape in order support improved hip health, maintain existing good health, prepare for or recover from surgery, our multidisciplinary team of experts is here to help. You can book an appointment with them directly, or request a call by completing the following form, so we can answer your questions and book a time to meet that suits you.